The purpose of this paper is to provide a summary of the evidence supporting the use of visible light, ultraviolet (UV) disinfection, local air filtration, and fumigation technologies to control the transmission of COVID-19. These key results are:
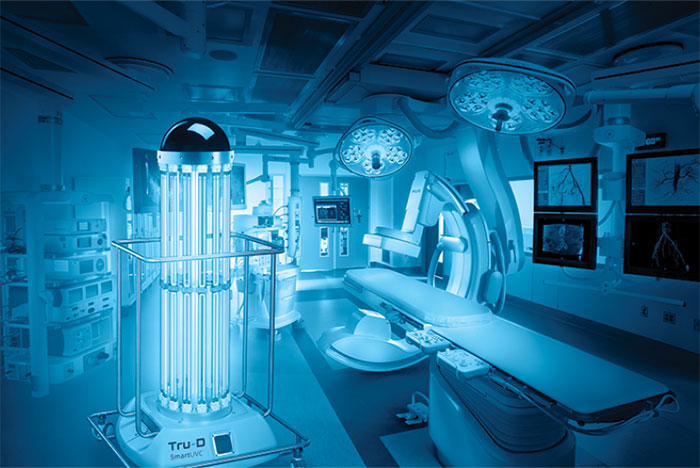
- There is a reasonable amount of data to suggest that germicidal UV (GUV) that makes use of UV-C light and fumigation techniques (especially Hydrogen Peroxide Vapour (HPV)) are likely to be successful decontamination approaches against SARS-CoV-2 for rooms that are vacant. Both are readily accessible as commercial systems and are already used for terminal disinfection in a variety of medical facilities. However, “shadowing” effects can also affect the efficacy of fumigation, with areas that are the most difficult to reach being those that are facing away from the delivery equipment or are located on the underside of room surfaces. UV-C is more difficult to apply effectively in a complex space with surfaces that are in shadow.
- Both decontamination methods, UV-C and fumigation, need to be applied for an adequate amount of time in order to be successful. As a result, they are more likely to be effective as a component of a terminal cleaning procedure rather than as a daily disinfectant due to the fact that they are concentrated. This is especially true for the process of fumigation, which requires a cycle duration of thirty to ninety minutes in addition to additional time for aeration to eliminate any surplus fumigants.
- UV carousel devices are commonly deployed for a period of time ranging from 20 to 45 minutes, depending on the size of the room to be treated. However, in order to counteract shadowing effects, relocating the device and repeating the treatment may be required.
- For methods of fumigation, the elimination of fumigant by aeration is a specific aspect that should be taken into consideration, in particular in settings that include a significant number of soft furnishings.
- Although there is limited evidence for use against respiratory viruses in a real-world setting, there is strong evidence that upper room GUV (as an air filtration system) has the potential to be used effectively to reduce microbial load in occupied rooms’ air. This is despite the fact that there is limited evidence. This technique can only be used in rooms that have ceilings that are sufficiently high, and it functions best in areas that have inadequate air circulation. Although it shouldn’t be considered as a replacement for ventilation, it might be useful in situations when that aspect of the environment can’t be addressed. A GUV system for an upper room has to have the appropriate dimensions for the size of the room as well as the microorganisms, and it also needs to take into account its interaction with the ventilation flow.
- Unless the airflow rate through the device is adequate, it is doubtful that local air cleaning devices, such as filter devices and UV-C devices, which may be found in combination, would have a major advantage. This is because filter devices and UV-C devices might be found in combination. There are likely some areas with inadequate ventilation that might benefit from having these installed.
- Far-ultraviolet technology shows promise as a control, but it is still at an extremely early stage of development to be used in real-world settings without much more study.
- Visible or blue/violet (HINS) light may reduce bacterial contamination in structures. There’s minimal proof the influence affects viruses. Increasing the natural light that enters a structure (by opening the curtains, for example) is a preventive strategy that incurs no expenses if there is already enough light, but the benefits are likely to be small. HINS light’s benefits need more study since it’s being employed in hospitals.
- Both the UV-C and the fumigation decontamination methods have significant safety considerations, and they should only be carried out by trained personnel who have appropriate risk assessments and controls in place.
- Significant safety factors must be taken into account throughout the design, installation, and operation of the upper room GUV. These considerations must be taken into account.
- We haven’t considered any of these techniques’ cost-effectiveness. This component must be studied in combination with conventional tactics, such as improving ventilation and increasing the quantity of regular cleaning procedures, to establish whether applying disinfection technology is beneficial.
- The techniques in this essay should not substitute comprehensive cleaning or ventilation. These technologies can only enhance existing methods; they can’t replace them. Despite what some providers may say, chemical fumigation and UV-based room treatments are disinfection techniques, not sterilizing methods. It’s crucial to distinguish.
Related Article: Learning to use and set up Surya Professional disinfectant with UV-C sterilizer box
ultraviolet disinfection methods for air filtration
UV radiation in the UV-C wavelength range (200 nm to 280 nm) is used in the technique of germicidal ultraviolet (GUV, also known as UVGI) to render bacteria inactive. The majority of systems use low-pressure mercury lamps, whose peak emission occurs at 254 nm. The method is widely used for water treatment, room decontamination, ventilation/coiling coil treatment, and in-room air disinfection as an inactivation technique.
Considerations for health and safety must be made while using UV-C for surface, air filtration, and air disinfection. As UV-C exposure may seriously harm a person’s eyes and skin, UV lamps must be installed inside of shielded or enclosed structures, or they must only be used when no one is around. Since double-glazed units often prevent the transmission of UV-C light from these devices in practice, the majority of the exposure risk is believed to be related to exposure to the irradiation effects that may be present in the space when a unit is turned on.
It is generally recommended to use UV-C devices in ventilation systems for buildings to prevent the spread of illness and minimize contamination of cooling coils, both of which improve energy efficiency. This strategy could be advantageous in commercial UK buildings, but because UK hospitals (with a few notable exceptions) have 100% fresh air ventilation systems, UV-C installation won’t help.
Research on the use of UV-C devices for airborne infection control is the primary focus of research on the upper-room GUV. These UV-C shielded machines produce an ultraviolet light band over the heads of the people within. Pathogens from the inhabited zone are transported through the upper-room UV zone by the airflow patterns inside the room, ensuring continuous disinfection while the room is occupied.
The method doesn’t completely disinfect the environment; rather, it reduces the concentration of pathogens in the air in the room, lowering the danger of transmission in a manner comparable to enhanced ventilation. This sort of device has a number of benefits over portable UVC carousels, including the treatment’s ability to keep the room busy.
With some material available in CIBSE Guide A, ASHRAE provides guidelines on GUV systems. CIE (2020) has also developed a policy statement on GUV that states that UV-C has considerable promise but may be dangerous and, as a result, must be implemented with caution. They advise utilizing only professionally built items that adhere to safety standards and point out the need for UV measurements for any partially enclosed systems to ensure that human exposure limits are not exceeded. It should be noted that the condition of the bulbs affects how well GUV systems work. UV-C lamps’ output deteriorates with time, and grime on the lamp’s surface also has an impact. The proper operation of a GUV system depends on good maintenance.
Related Article: Is UV-C light harmful for air ducts and electronics?
approaches using different light wavelengths
Since it is already known that SARS-CoV-2 decays quickly in direct sunshine, it is debatable whether it would be useful to merely increase light levels in constructed environments. The evidence for the effects of sunlight and natural ventilation (the “open air factor”) on microorganisms is reviewed by Hobday and Dancer (2013) and includes a number of earlier studies.
Numerous studies are cited to demonstrate that bacteria exposed to direct sunlight, even through a window, are rendered inactive, whereas bacteria exposed to diffuse light can persist for longer periods of time. There don’t seem to be any recent studies on this topic or studies on viruses, and the majority of studies date back more than 40 years. However, a review paper on buildings and COVID-19 suggests that one easy step that might have an impact is opening blinds to let more light into buildings.
Related Article: What UV light is best for plants
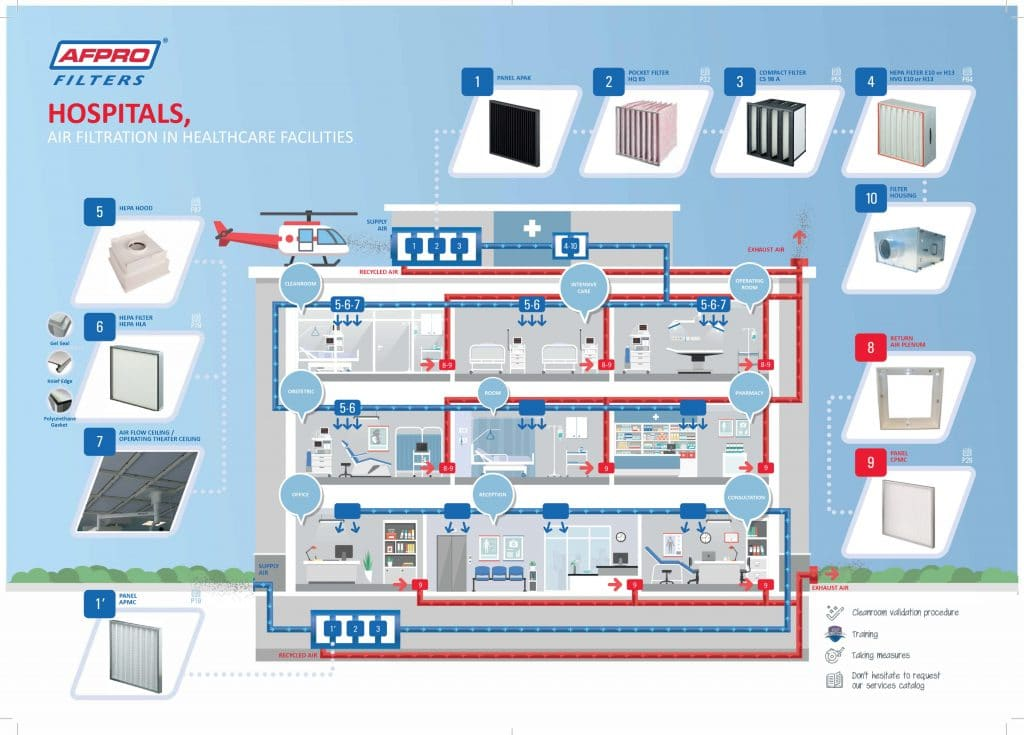
Healthcare uses air filtration technology
An evaluation of the usage of a portable air filtration system in hospital pediatric treatment areas was conducted by Rao et al. in 2020 healthcare research. The usage of a system using photo-electrochemical oxidation (PECO) technology was assessed in this prospective research. A matched patient population made up the historical control group; 273 were hospitalized in the preintervention period (control group) and 289 in the postintervention phase (where air purification was used). The average amount of time spent in the ICU dropped from 0.7 days before the intervention to 0.4 days after treatment (those in rooms treated with an air filtration).
The average number of days spent in the hospital decreased by 0.3. In the pre-intervention phase, 77 percent of patients used non-invasive ventilation; in the post-intervention period, that number dropped to 23 percent. Pre-intervention nebulizer usage was 59 percent, while post-intervention nebulizer usage was 41 percent. Intubations were performed at a rate of 57.1 percent prior to intervention and 43 percent following it. The authors came to the conclusion that portable PECO air filtration may shorten hospital stays, lower intubation rates, and lessen the requirement for nebulizers and noninvasive treatment for pediatric patients who are hospitalized with respiratory distress.